Medicare Reimbursement Cuts and W-RVU Increases
CMS announced its plans to revalue the office and out-patient (OP) Evaluation and Management (E/M) code several years ago. Since the CMS Medicare “pie” is $1.00, if there are increases for the office and OP E/M services, there must be corresponding cuts elsewhere under Congressionally mandated “budget neutrality.” Both ACEP and EDPMA have filed multiple comment letters requesting that the work value (W-RVU) of the ED E/M codes should be increased to keep the parity that has existed between these codes and the office codes since the creation of RBRVS in 1992.
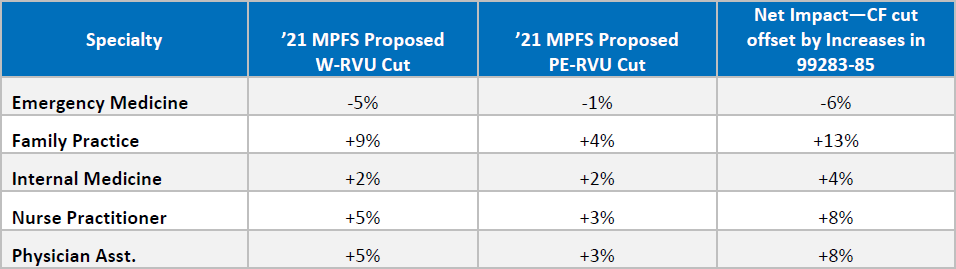
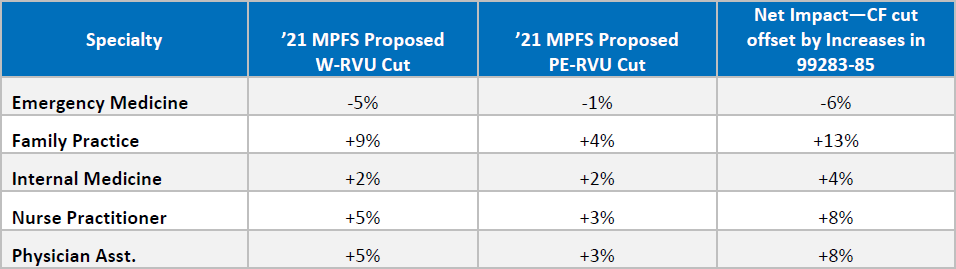
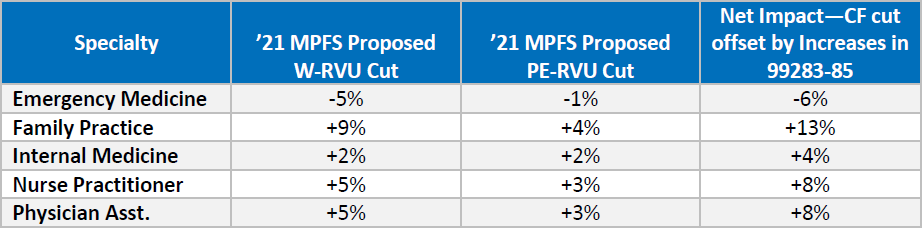
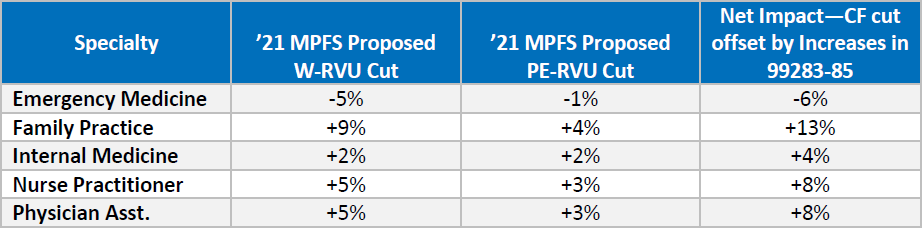
While those requests for increases in the W-RVUs for CPTs 99283-85 were agreed to by CMS in this PFS proposed rule (see detail below); the -10.6% reductions in the conversion factor (CF) overcame the E/M increases and emergency medicine (EM) netted a -6% for 2021.
The Case for Telehealth (T/H) has been made by COVID-19:
T/H has for years shown great clinical and potential savings promise but has been hampered by reimbursement requirements that severely limited its potential– that all changed with the global pandemic. With an effective date of March 1, 2020, the HHS Secretary declared a public health emergency (PHE) and now has the legal authority to waive the T/H restrictions under a separate statute authorizing the PHE declaration. CMS has agreed that the ED E/Ms would be reimbursed, retroactive to March 1, 2020. The statutory “originating” and “distant” site requirements were suspended. Important to note, once the PHE has been lifted—the current declaration expires Oct. 23, 2020—the T/H reimbursement restrictions on the originating and distant site will be restored.
2021 Medicare Physician Fee Schedule (MPFS) 2021 Proposed Rule Summary
On August 3, 2020, the Centers for Medicare & Medicaid Services (CMS) released a Medicare annual payment rule for calendar year (CY) 2021 that impacts payments for physicians and other clinicians. The rule combines proposed policies for the Medicare physician fee schedule (MPFS) with those for the Quality Payment Program (QPP)—the performance program established by the Medicare Access and CHIP Reauthorization Act (MACRA). Comment letters are due to CMS on October 5, 2020.
Conversion Factor:
CMS’ decision from last year’s rule to increase the office and outpatient evaluation and management
(E/M) services in 2021, as well as other technical refinements, results in a significant “budget neutrality” adjustment to the conversion factor. The budget neutrality requirement forces CMS to make an overarching negative adjustment to physician payments in order to counterbalance any increases in code values that CMS implements. CMS usually does this by adjusting the Medicare “conversion factor”—which converts the building blocks of PFS codes (relative value units or RVUs) into a dollar amount.
The significant increases in the office and outpatient E/M values that CMS previously finalized for 2021 leads to a significant downward adjustment to the conversion factor, requiring an offset of around $5.5 billion. To preserve budget neutrality, CMS is proposing to reduce the conversion factor by -10.6 percent in 2021 from $36.09 to $32.26 —dropping it to one of the lowest levels it has been in 25 years.
Emergency Medicine Reimbursement and Emergency Department (ED) E/M services: The cut to the CF will reduce reimbursement levels for all physicians and other health care practitioners. However, the actual impact of the cut on reimbursement depends on the codes that the physicians and other health care practitioners typically bill. As seen below, the total payment clinicians receive for a service depends on both the amount of RVUs for the service and the size of the conversion factor (as well as a geographic adjustment).
Total payment under the MPFS = total RVUs x geographic adjustment x conversion factor
For specialties that primarily bill the office and outpatient E/M codes, the magnitude of the increase in these code values outweighs the cut to the CF—so overall these clinicians will expect to see an increase to their reimbursement.
ACEP and EDPMA knew that the office and outpatient E/M policy would cause a significant across the board reduction in payment in CY 2021 and therefore made it a priority to offset some of that cut for ED. Being the sole representative for ED at the AMA/RUC (RVS Update Committee), ACEP argued for CMS to increase the value of the ED E/M codes to appropriately align with the revised office and outpatient E/M code levels for new patients. In the rule, CMS is proposing to accept ACEP’s recommendation, and increase ED E/M codes to match the values that we had specifically advocated for (found below):
Work RVU Changes
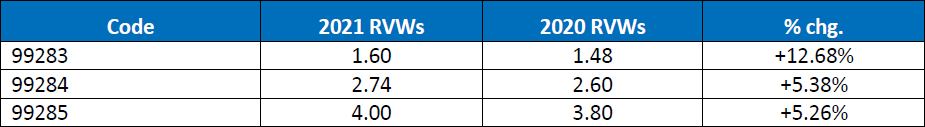
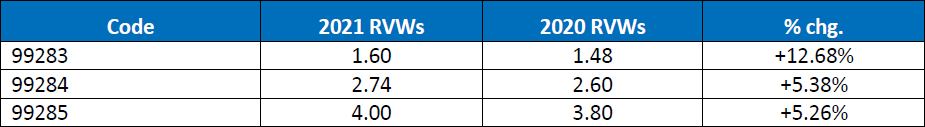
According to CMS, the increase in the value of these codes will cause the payments to bump up by approximately 3 percent. After considering this increase and other adjustments, the overall reduction to emergency medicine is expected to be -6 percent, significantly less than the 10.6 percent cut to the conversion factor. All in all, emergency physicians received a raise, but CMS’ budget neutrality rules cancelled it out.
It is important to remember that this is a proposed rule, and in the formal comments on the rule, ACEP and EDPMA will urge CMS to do everything that it can to mitigate the impact of the budget neutrality adjustment to the conversion factor. The letter expresses strong concerns on this proposed cut and notes the unprecedented strain emergency physician practices already are facing due to the ongoing COVID-19 pandemic. If Congress acts, emergency medicine reimbursement would increase by around 4-5%, instead of decrease by 6%.
Telehealth Services:
During the COVID-19 public health emergency (PHE), CMS took numerous steps to expand the use of telehealth under Medicare. ACEP’s fact sheet. Specifically, CMS temporarily added many codes, including all five ED E/M codes (CPT codes 99281 to 99295) to the list of approved telehealth services. That means that these codes are reimbursable under Medicare when performed remotely via telehealth at the same rate as they are when the services are delivered in-person. CMS used its unique “1135” waiver authority that only exists during a national emergency to temporarily waive two existing telehealth restrictions: the originating site requirement, which mandates that Medicare beneficiaries receive a telehealth service from a certain type of health care facility and not from any location like their home; and the geographic requirement, which restricts telehealth in Medicare to only rural areas.
Waiving these requirements during the PHE allows clinicians to perform telehealth services regardless of where they or their patient are located as well as in both urban and rural areas. These waivers have significantly expanded the use of telehealth during the pandemic. In fact, on the same day that the rule was released, President Trump signed an Executive Order asking that CMS issue a rule that examines, which additional telehealth services should be offered to Medicare beneficiaries.
Three Categories: In the proposed rule, CMS breaks out the codes that it temporarily added to the list of approved telehealth services into three categories:
Category 1: Codes that CMS is proposing to be included on the list of approved telehealth services permanently;
Category 2: Codes that CMS is proposing to be included on the list of approved telehealth services for the remainder of the calendar year in which the PHE ends (i.e. if the PHE ends in January 2021, the codes would remain on the list until December 31, 2021);
Category 3: Codes that CMS is proposing to be removed from the list of approved telehealth services once the PHE ends
CMS is proposing to only include those codes that are similar to office-based codes that are already permanently approved in Category 1. However, CMS is proposing to include the ED E/M codes levels 1-3 (CPT codes 99281-99283) in Category 2, which means they are at least temporarily added to the list for a period of time after the PHE ends. CMS states in the rule that it believes that these codes have the potential to add clinical benefit outside of the PHE and could therefore be added to the list permanently. However, CMS is looking for additional information from the public that would supplement its clinical assessment of these codes.
CMS is proposing to place ED E/M codes levels 4 and 5 (CPT codes 99284 and 99285) as well as hospital, intensive care unit, and observation stays and critical care services (CPT codes 99217-99220; 99221-99226; 99484-99485, 99468-99472, 99475- 99476, 99477- 99480, and 99291-99292) in Category 3. CMS is concerned that these services cannot truly be performed via two-way, audio/video telecommunications technology, due to the characteristics of patients who receive the services, the clinical complexity involved, the urgency for care, and the need for complex decision-making. Although CMS is proposing not to add these codes to the list of approved services past the end of the PHE, it is seeking comment on whether any of these codes should be shifted to category 2.
Audio-only Codes – CMS is not proposing to continue to include telephone codes (audio-only) on the list of approved telehealth services past the PHE. CMS states that it does not have the authority to waive the requirement that telehealth services include both an audio and visual requirement. However, CMS is seeking comment on whether the agency should develop coding and payment for a service similar to the virtual check-in but for a longer unit of time and with an accordingly higher value. CMS is also seeking comment on whether separate payment for such telephone-only services a provisional policy should be to remain in effect until a year or some other period after the end of the PHE or if it should be PFS payment policy permanent.
Direct Supervision – Many services under the PFS can be delivered by auxiliary personnel under the direct supervision of a physician. In these cases, the supervision requirements necessitate the presence of the physician in a location, usually in the same location as the beneficiary when the service is provided. During the PHE, CMS is temporarily modifying the direct supervision requirement to allow for the virtual presence of the supervising physician using interactive audio/ video real-time communications technology. In the rule, CMS is proposing to extend this policy until the later of the end of the calendar year in which the PHE ends or December 31, 2021. CMS will solicit public input on circumstances where the flexibility to use interactive audio/video real-time communications technology to provide virtual direct supervision could still be needed and appropriate.
Clarification of Current Telehealth Rules – Finally, CMS is clarifying under existing telehealth rules that “incident-to” services may be provided via telehealth if they are under the direct supervision of the billing professional. CMS is also clarifying that clinicians are allowed to use telehealth equipment to provide a service to a patient in their same location, but the service should not be billed as a telehealth service.
Scope of Practice: CMS is proposing to allow nurse practitioners (NPs), clinical nurse specialists (CNSs), physician assistants (PAs) and certified nurse-midwives (CNMs) to supervise the performance of diagnostic tests in addition to physicians. CMS granted this flexibility during the pandemic and is now proposing to extend it permanently. CMS is concerned about ensuring an adequate workforce in areas where there are shortages and seeks information states that have scope of practice laws.
MPFS Payment for Services of Teaching Physicians: CMS is seeking comment on whether to permanently extend the policy instituted during the COVID-19 PHE that allows teaching physicians to supervise residents remotely using telehealth (audio-visual) equipment as mentioned above. There is also consideration to extend the temporary waiver to allow residents to “moonlight” in the inpatient setting.
Medical Documentation Requirements: In last year’s rule, finalized numerous changes to the medical record documentation requirements for physicians and other health care practitioners. In this proposed rule, CMS is clarifying that physicians and other health care practitioners, including therapists can review and verify documentation entered into the medical record by members of the medical team for their own services that are paid under the MPFS.
Appropriate Use Criteria Program: While the proposed rule does not discuss the AUC program, CMS announced on Aug. 10 that the educational and operations testing period will be extended through 2021. As a result, there are no payment consequences associated with the AUC program for 2021, and instead CMS encourages providers to use 2021 to learn, test, and prepare.
Payment for Medication Assisted Treatment (MAT) in the ED: Based on the advocacy of ACEP and EDPMA, CMS is proposing to pay for MAT delivered in the ED starting in 2021. Specifically, CMS is proposing to create an add-on code to be billed with E/M visit codes used in the ED setting. This code would include payment for assessment, referral to ongoing care, follow-up after treatment begins, and arranging access to supportive services. The add on code would have a work RVU value of 1.30, which is between a 99282 and 99283 (ED E/M code levels 2 and 3).
Electronic Prescribing of Controlled Substances: CMS is implementing a provision of the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities
(SUPPORT) Act, which requires electronic prescribing of controlled substances (EPCS) under Medicare Part D. CMS is proposing to require EPCS by January 1, 2022 to allow for sufficient time to implement feedback from the Request for Information and to help ensure that the agency is not burdening providers during the current public health emergency for the COVID–19 pandemic.
Medicare Coverage for Opioid Use Disorder (OUD) Treatment Services Furnished by Opioid Treatment Programs (OTPs): In last year’s rule, CMS implemented a new Medicare benefit for the treatment of opioid use disorder furnished by OTPs. In doing so, CMS established new codes describing the bundled payments for certain episodes of care that include methadone, oral buprenorphine, implantable buprenorphine, injectable buprenorphine or naltrexone, and non-drug episodes of care, as well as add-on codes for intake and periodic assessments, take-home dosages for methadone and oral buprenorphine, and additional counseling. In this year’s rule, CMS is proposing several refinements to the new benefit. One of the proposals is to expand the definition of OUD treatment services to include opioid antagonist medications, such as naloxone. It is important to remember that this benefit only applies to services delivered by OTPs. ACEP believes that at least some of these services should also be paid for when delivered in the ED, such as the administration of naloxone.
Learn more about Zotec Partners here.